Can stress really cause stomach ulcers? What about spicy food and coffee?
The two proven causes of stomach ulcers are bacteria and painkillers, specifically non-steroidal anti-inflammatory (NSAID) drugs such as aspirin and ibuprofen. Find out why.

(Photos: iStock/duoma and Stanislav Tarasov)

This audio is generated by an AI tool.
Here’s a question: What do you think causes stomach ulcers? If you think it’s spicy food, salty food, coffee, alcohol or stress, the answer is, well, “yes” and “no” (more on that in a bit).
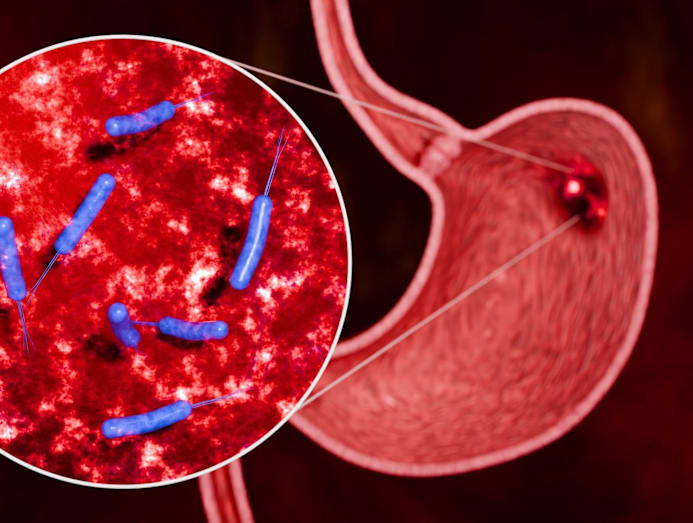
What's for certain is that stomach ulcers are caused by catching the Helicobacter pylori bacteria or H pylori for short.
These hardy organisms are specially adapted to living in the highly acidic environment of the stomach lining, said Dr Reyaz Singaporewalla, a senior consultant endocrine and general surgeon at ACE Specialist Surgery & Endoscopy. “The bacteria produce an enzyme called urease, which creates a more alkaline micro-environment around itself. This helps it buffer acid and survive,” he explained.
This urease is what triggers inflammation of the stomach, leading to what we know as chronic gastritis, explained Dr Melvin Look, a consultant gastrointestinal surgeon with PanAsia Surgery. “It weakens the lining of the stomach and the stomach acid may eventually erode the lining of the stomach to form ulcers.”
And just to make sure the bacteria hangs in there, evolution has endowed H pylori with a “tail-like structure called flagella, which it uses to burrow into the mucus layer of the inner stomach lining", added Dr Look.

HOW IS THE BACTERIA TRANSMITTED?
Transmission is most commonly linked to shared eating practices, and poor hand hygiene and sanitation habits rather than any single action, said Dr Singaporewalla. Incriminating actions can include tasting food from the same bowl or close physical contact involving saliva. “Poor hand hygiene before meals or food preparation can also increase the risk of faecal-oral spread.”
The bacterial spread can just as likely occur during childhood, said Dr Chua Tju Siang, a senior consultant gastroenterologist with AliveoMedical. “Less commonly, it can spread through exposure to vomit or by adults chewing food before feeding infants.”
Now surely, the temperature and spiciness of certain food such as piping-hot mala hotpot, or the fiery chilli burn of sambal can destroy the nasties? Unfortunately, no.
“Boiling temperatures can kill many organisms, in principle, but hotpot dipping is not a controlled sterilisation step,” said Dr Singaporewalla. There are many factors involved such as “insufficient contact time, re-contamination from saliva, and the part of the utensil that touches the mouth may not be adequately dipped”.
Furthermore, “festive gatherings, where families eat together over long meals and shared dishes, can increase exposure, especially when hygiene routines become more relaxed”.
Choosing a spicy broth or dipping food into sambal is not a solution either. Spicy foods do not disinfect utensils, said Dr Chua. “Spiciness comes from chili compounds such as capsaicin, which may cause irritation, but does not have sufficient anti-bacterial effect at the concentrations found in food to kill H pylori.”
5 TIPS TO AVOID SPREADING ULCER-CAUSING BACTERIA
- Use serving utensils for shared dishes, recommended Dr Reyaz Singaporewalla, a senior consultant endocrine and general surgeon at ACE Specialist Surgery & Endoscopy. "Make it a norm, not a 'someone is sick' rule."
- Avoid double-dipping tasting spoons during cooking. "Use a clean spoon each time or portion out to taste," said Dr Singaporewalla.
- Practise good hand hygiene, especially before meals, advised Dr Chua Tju Siang, a senior consultant gastroenterologist with AliveoMedical. "Regular handwashing with soap after using the toilet and before eating is one of the most effective ways to reduce faecal–oral transmission."
- Don’t share drinks, straws, bottles, cups and anything that touches the lips.
- Thoroughly wash raw vegetables and fruit to clear all traces of fertilisers and contaminants before consumption, said Dr Melvin Look, a consultant gastrointestinal surgeon with PanAsia Surgery.
HOW LONG DOES THE BACTERIA TAKE TO DEVELOP STOMACH ULCERS? WHAT ABOUT CANCER?
“There is no set timeline for stomach ulcers to form after H pylori infection,” said Dr Chua. “Whether an ulcer develops depends on factors such as how aggressive the bacterial strain is, your genetic make-up and lifestyle factors like smoking or frequent painkiller use.”
In fact, many people contract H pylori and don't ever develop ulcers, said Dr Singaporewalla. “Across populations, the lifetime risk of peptic ulcer disease among those infected is often quoted around 10 per cent to 20 per cent, meaning most infected individuals do not develop ulcers. In those who do, it usually happens after a prolonged period of inflammation, often months to years.”
Still, H pylori is not to be taken lightly. Often, cancers in the lower part of the stomach are caused by chronic H pylori infection in 90 per cent of cases, said Dr Look.
“H pylori is a very common infection in Singapore and parts of Asia such as Vietnam and China," continued Dr Look. "In 1994, it was classified as a Class 1 carcinogen by the World Health Organization, making it the only bacterium recognised to be a definite cause of cancer in humans as it is specifically linked to development of stomach cancer and stomach lymphoma.”
The good news is, despite the strong association between H pylori and stomach cancer, only 1 per cent to 3 per cent of infected people will eventually develop cancer after harbouring the infection for many years, said Dr Look.
SO, STRESS ISN’T THE CAUSE OF STOMACH ULCERS THEN?
The two major proven causes of stomach ulcers are H pylori and painkillers, specifically non-steroidal anti-inflammatory (NSAID) drugs such as aspirin and ibuprofen, said Dr Singaporewalla.
NSAIDs damage the stomach by blocking prostaglandins, natural substances that protect the stomach lining by maintaining mucus production and blood flow, explained Dr Chua. “The risk of ulcers increases with higher doses, use beyond seven to 14 days, age or a history of ulcers.” In susceptible individuals, “even a single dose of NSAID can cause an ulcer, albeit uncommonly”, he added.
As for stress, “everyday psychological stress does not directly cause peptic ulcers in most people”, said Dr Singaporewalla. But what chronic mental stress can do is delay ulcer healing and encourage behaviours that raise ulcer risks, such as smoking, alcohol and painkiller use, highlighted Dr Chua. “So, stress is a contributor, not a primary cause, in most people.”
BUT WHAT IF YOU NEED TO TAKE PAINKILLERS?
A better alternative is paracetamol. “In selected patients, COX-2 inhibitors, such as etoricoxib and celecoxib, may be considered,” said Dr Chua. “Although COX-2 inhibitors are considered more ‘stomach-safe’, they can still cause ulcers – just at a lower risk than traditional NSAIDs.” If NSAIDs or COX-2 inhibitors are unavoidable, adding stomach-protective medications such as proton pump inhibitors is often recommended, he said.

WHAT ABOUT CERTAIN FOOD AND DRINKS? CAN THEY CAUSE STOMACH ULCERS?
Spicy and acidic food as well as caffeine aren’t direct causes of stomach ulcers, concurred the gastro experts. But they can irritate an already inflamed stomach lining and make other digestion symptoms feel worse, said Dr Singaporewalla. Caffeine, for example, may worsen indigestion or reflux symptoms in some individuals, he said.
When it comes to smoking, alcohol and too much salt in your diet, the damage hits you in the stomach more directly. “Smoking, alcohol and an excessive intake of salt can cause stomach ulcers by their direct injury to the stomach lining,” said Dr Look. For instance, a high salt intake damages the stomach’s protective mucus and renders the stomach more vulnerable to inflammation by gastric acid and/or H pylori, explained Dr Chua.
As for alcohol, it can irritate the stomach lining, and worsen gastritis and ulcer symptoms, according to Dr Singaporewalla. “Having five or more drinks a day significantly increases the risk of bleeding from an existing ulcer,” added Dr Chua. “If you have ulcer symptoms, it’s best to avoid alcohol until assessed or healed,” advised Dr Singaporewalla.

As for smoking, it “impairs the body's ability to heal existing ulcers and significantly raises the likelihood that ulcers will return even after treatment”, said Dr Chua. “Furthermore, it is a major confirmed risk factor for stomach cancer, making it a critical habit to break for long-term gastric protection.”
WHAT ARE THE SIGNS OF AN H PYLORI INFECTION?
“Many people infected with H pylori have no symptoms at all. When symptoms do occur, they are usually related to stomach irritation or ulcers,” said Dr Chua.
According to Dr Singaporewalla, symptoms that possibly point to an ulcer include the following. “If symptoms persist beyond a few weeks or recur repeatedly, medical evaluation and testing may be appropriate.”
- Upper abdominal discomfort or burning
- Bloating or early fullness
- Nausea
- Frequent burping
- Recurring indigestion

When a stomach ulcer develops, said Dr Look, the mild discomfort can become more intense and persistent. “The pain may wake you up at night or it can penetrate posteriorly towards your back. Ulcers can start to bleed, so you may vomit blood or pass black, tarry blood in your stools.”
Other more serious symptoms include unexplained weight loss or anaemia, which may indicate complications and medical evaluation should be sought, advised Dr Chua.
If you have been found to be infected, said Dr Look, “it is usually a good idea to consider testing your close contacts, especially family members who often share food together”.
“Testing and treating family members can help them eradicate H pylori before it can cause problems such as ulcers and stomach cancer. It can also help to prevent them from spreading the infection back to you after you have been treated successfully.”

WHAT DOES TREATMENT INVOLVE?
At least two types of antibiotics are prescribed to eradicate the H pylori bacteria, explained Dr Singaporewalla.
A proton pump inhibitor (PPI) is often added to reduce acid production in the stomach, and help heal any existing ulcers; if the patient can’t tolerate PPI, histamine receptor blockers may be prescribed instead. “Bismuth subsalicylate can be added to promote the healing of the stomach lining when necessary,” said Dr Singaporewalla.
“Completing the full course as prescribed is important for successful eradication,” he emphasised.
CAN DIET ALONE ERADICATE THE BACTERIA?
Sorry but no, said the gastro experts. “Diet changes alone are not reliable for eradication because H pylori is adapted to persist in the stomach lining,” said Dr Singaporewalla. “While dietary changes may reduce symptoms, inflammation or bacterial activity, they do not fully kill the bacteria,” added Dr Chua.
You could give certain foods a shot such as probiotic-containing yoghurt and milk drinks; antioxidant-rich and inflammation-quelling fruits and vegetables (berries, broccoli, leafy greens and citrus fruits are good options); polyphenol-containing green tea; and antimicrobial herbs and spices such as garlic.
“While these foods can support stomach health and may slightly reduce bacterial levels, they are not strong or consistent enough to eradicate the infection on their own,” qualified Dr Chua.






