Afraid of needles? Tips to ease your anxiety whether you’re drawing blood, getting an injection or doing Botox
It’s not personal if the nurse isn’t using the thinnest needle on you. Find out why certain needle thicknesses are needed and how you can make the procedure less painful.

(Photos: iStock/golfcphoto)

This audio is generated by an AI tool.
No one likes needles. But there are times when they do get under your skin, quite literally, like during vaccination, having your blood drawn for a health check, or getting an aesthetic procedure such as Botox or dermal fillers. That’s when you might be reduced to a pile of sweaty pits and clammy palms in the doctor’s office. But take it from the folks who draw blood for a living or phlebotomists in medical speak: You’re not alone.
“I’d say about one in 10 adults shows some degree of needle anxiety,” said healthcare organisation SATA CommHealth’s senior staff nurse Nur Ain Mohd Basir. “It’s quite common even among those who’ve had injections or blood tests before,” she added. “Some become tense or anxious the moment they see the needle, while others may just need some reassurance.”
While not everyone has a full-blown phobia of needles, many do feel faint, anxious or uneasy, said a spokesperson from National University Hospital’s (NUH) Department of Laboratory Medicine. Interestingly, they noticed that patients needing medical care tend to manage their nerves better than those who voluntarily donate blood.
If your appointment is coming up and you’re feeling prickly about getting poked, knowing the "why" behind the choice of needles used, and what you can ask for can help make those moments less anxious.

WHY CAN’T THEY SIMPLY USE THE THINNEST NEEDLE?
That’s because it depends on the viscosity of the injected material, and where the needle needs to reach to deliver it.
Generally, shorter and thinner needles are used for subcutaneous injections meant to reach just under the skin. These needles are also prepped for medications with thinner consistencies, such as insulin, GLP-1 receptor agonists for weight management, allergy shots and even Botox.
Intramuscular jabs that hit the muscles (including influenza and COVID-19 vaccines) typically require longer and thicker needles, according to GoodRx. A thicker needle would also work better at delivering medications that are formulated to be viscous and slowly absorbed such as certain hormone therapies or long-acting antipsychotic.
You’ll also have to tolerate a slightly thicker needle during blood drawing or venipuncture to minimise haemolysis risk or the rupturing of your blood cells, explained NUH’s spokesperson. Your blood cells can be sheared by a too-thin needle and this can affect your blood test results.
Fillers, too, especially viscous hyaluronic acid ones, may require a thicker needle for the product to flow smoothly.

WHY IS IT ALWAYS THE SAME FEW INSERTION SITES?
The upper arm is often the site for injections because the deltoid muscle there can keep the vaccine localised for a while. This creates enough time for the deltoid’s immune cells (yes, muscles have immune cells, too) to sound the alarm to other immune cells to get to work, explained Associate Professor of Nursing Libby Richards from Purdue University in The Conversation.
Plus, the vaccine doesn’t have to travel far to reach the lymph nodes – the key players of your body’s immune system – that lie just under the armpit, she wrote.
When it comes to blood drawing, the median cubital vein located in the bend of your arm is a more stable (less likely to roll) and juicy vein that ticks the phlebotomist’s boxes. It also lies closer to the skin’s surface, making it easier to find after applying a tourniquet. And apparently, the skin covering that area is less sensitive than the skin overlying other veins, according to Medscape.
As for Botox and filler injections, the sites would depend on your aesthetic needs as discussed with your doctor.
SO, WHAT TYPE OF NEEDLE IS USUALLY USED?
A needle’s thickness is known as the gauge and is listed as “G” on the label. “The gauge system is inversely proportional; the higher the gauge number, the smaller the needle’s diameter,” said the NUH spokesperson. For example, a 31G needle is thinner and has a smaller diameter than a 28G one.

Meanwhile, the length of a needle is indicated as a number next to the “G”, usually in fractions of inches. Needle lengths can vary widely, said the NUH spokesperson, from 3/8 inch for subcutaneous needles to three inches for very deep intramuscular needles. (An inch is about 2.54cm.)
According to NUH, subcutaneous jabs can be performed with 25G to 32G needles with lengths of 3/8 inch (about 1cm) to 5/8 inch (about 1.5cm). For intramuscular injections, 21G to 25G needles that are between one and 1.5 inches are preferred.
For comparison, a 25G needle has an external diameter of 0.5mm, while a 21G needle has an external diameter of 0.8mm to 0.85mm.
For routine blood drawing, phlebotomists generally use 21G to 23G needles, depending on the size of the patient’s veins, said NUH’s spokesperson. When the vein is extremely small or fragile, a butterfly needle may be used instead. It is so named for the plastic, wing-like flap on each side of the needle for better control during insertion.
When it comes to injectable aesthetic treatments, 30G needles are the gold standard for Botox, while a 22G to 25G needle may be used for viscous fillers, and a 27G to 30G one for thinner fillers.
CAN YOU ASK FOR A THINNER NEEDLE?
Of course, said Marissa Cruz Advincula, the nurse manager at SATA CommHealth’s Fernvale Dialysis Centre. “Patients can definitely let us know if they’re worried about pain or prefer a smaller needle. For injections or IV drips, we’ll try to use a smaller gauge if it’s suitable.”
However, for other procedures such as blood donation, dialysis and chemotherapy, you may be denied that request. “Specific needle sizes must be used to ensure proper flow and prevent complications,” said Advincula, especially for dialysis.
For renal patients, she said, a smaller needle size is not possible as a certain needle gauge (ranging from 17G to 14G) is required to deliver the prescription and ensure smooth blood flow.
The silver lining for patients requiring dialysis is plastic cannulas are now used in place of metal needles. “Plastic cannulas are more flexible and cause less discomfort when patients move their arms,” said Advincula. “They are suitable for patients with problematic or small veins, and help reduce complications such as aneurysms, which are more common with metal needles.”
You could also ask for a thinner needle at the aesthetic clinic but again, it depends on the injected product's viscosity. For Botox, there is the 34G "invisible needle", which is purportedly 33 per cent thinner than a 30G needle.
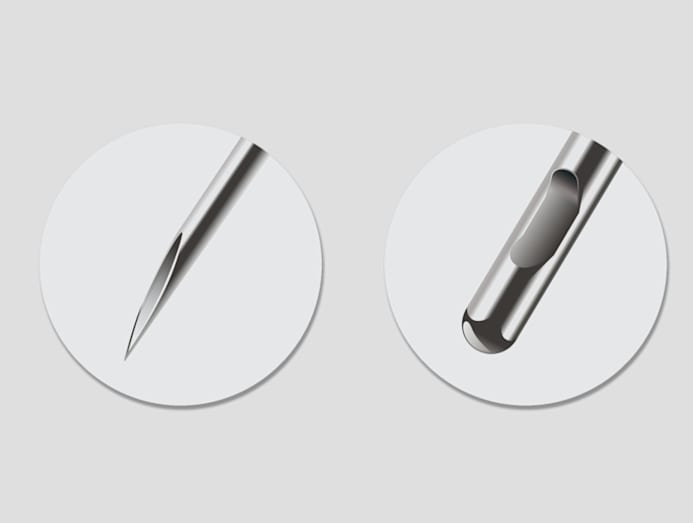
Another option to explore is the microcannula, a blunt-tipped metal tube that allows the aesthetic doctor to treat a large area with just one insertion point instead of multiple needle pricks.
WHY IS THERE A NEED TO RE-INSERT THE NEEDLE SOMETIMES?
No one wants to be treated like a human pin cushion. Unfortunately, re-inserting the needle is sometimes necessary during blood drawing if the vein is small, moves or collapses, said Nur Ain.
“I’ve had cases where the vein looked good at first but rolled slightly when the needle went in. When that happens, I always pause, explain to the patient what’s going on, and reassure the patient before trying again. Usually, once they relax and I adjust the angle, or choose another site, it goes smoothly,” she said.

WHY ARE SOME NURSES BETTER AT INSERTING THE NEEDLE THAN OTHERS?
It all boils down to experience, said NUH’s spokesperson. “The smoother the technique, the less you will feel it. More experienced phlebotomists know how to find the vein quickly, insert confidently, and minimise discomfort.”
Speaking of visible veins, not every vein that looks prominent is ideal for drawing blood, said the spokesperson. “We usually go by experience and feel; we gently press or palpate to check if the vein is springy, stable, and well positioned. Size, depth and movement all matter.”
In case you're wondering, phlebotomists train on real people, not dummies. "We work with volunteers and patients to get the technique right. Their willingness helps make us better, which in turn, benefits future patients," said the spokesperson.
CAN YOU MAKE BLOOD DRAWING MORE COMFORTABLE FOR YOURSELF?
“Staying hydrated really makes a difference,” said Nur Ain. “Drinking enough water the day before and on the day itself helps the veins become fuller and easier to locate. Avoiding caffeine and alcohol also helps since these beverages can dehydrate the body.”
But what if you were told to fast beforehand? “For most fasting blood tests, patients are allowed to take small sips of plain water,” said Nur Ain. “When someone comes in very dehydrated, especially if they haven’t had any water at all, their veins can be harder to access and the person may feel more anxious or light-headed.”
And there's good reason for the room to be slightly warm as strong air-conditioning can cause veins to contract. It also helps for you to stay relaxed, said NUH's spokesperson. “Tension can tighten muscles and veins.”






